As the body of research supporting the use of 3D radiography in orthodontics grows and the price of 3D CBCT technology wanes, many orthodontists find themselves asking an important question: Is 3D cephalometry right for my practice? Drs Katherine Kula and Ahmed Ghoneima, editors of the new book Cephalometry in Orthodontics: 2D and 3D, break down the decision-making process that practice owners should use to determine whether to upgrade to the third dimension.
3D imaging produces the most accurate representation possible, one that most closely matches our patients’ anatomy and the anatomical truth.
“3D imaging significantly improves the diagnostic value of imaging in orthodontics,” adds Dr Ghoneima, BDS, PhD, MSD. “Advances in 3D imaging software programs have improved our ability to determine different treatment options, monitor changes over time, measure treatment outcomes more accurately, and predict and display the final treatment results. 3D imaging provides clear images with easily identifiable anatomical landmarks. It produces the most accurate representation possible, one that most closely matches our patients’ anatomy and the anatomical truth.”
When 3D CBCT technology first hit the market, it came with a price tag that made it largely inaccessible to most practitioners and their patients. However, recent innovations to the technology have focused on minimizing the impact of initial drawbacks such as the price of the machines and the amount of radiation used. These improvements make now the perfect time for orthodontists to begin considering adding this technology to their practice or upgrading to a dual-capability machine with both 2D and 3D sensors.
“Practitioners who already have radiography equipment in their practice should consider if the equipment is aging and may need replacement in the relatively near future,” Dr Kula advises. “In addition to speaking with company representatives, they should talk to other clinicians who currently have 3D CBCT machines in their practices. Even if your office’s current 2D radiographic equipment still has considerable life, it doesn’t hurt to start asking these questions now so you’ll be prepared in the future. It is also important to consider that for the new orthodontist who is just starting a practice and is particularly conscious of cost, a financial investment in 2D-only radiographic equipment makes it especially onerous to add or replace it with 3D-capable equipment in the near future.”
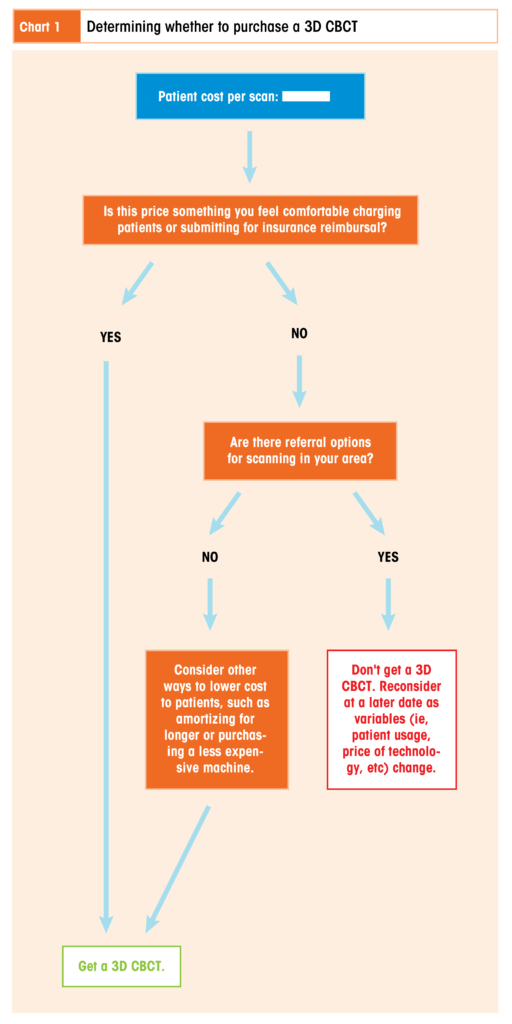
So how do clinicians decide whether to expand their practice’s capabilities to include 3D radiology? The list of questions curious clinicians should ask themselves is long: How many patients do you see who could benefit from having CBCT scans taken? How close is your current 2D radiographic equipment to needing replacement? How much does the unit you want cost, and how affordable will that cost be when it trickles down to your patients? Are there other local options for imaging to which you could refer your patients? The next sections will help you answer these questions and determine how you can incorporate 3D radiography into your practice.
Usage
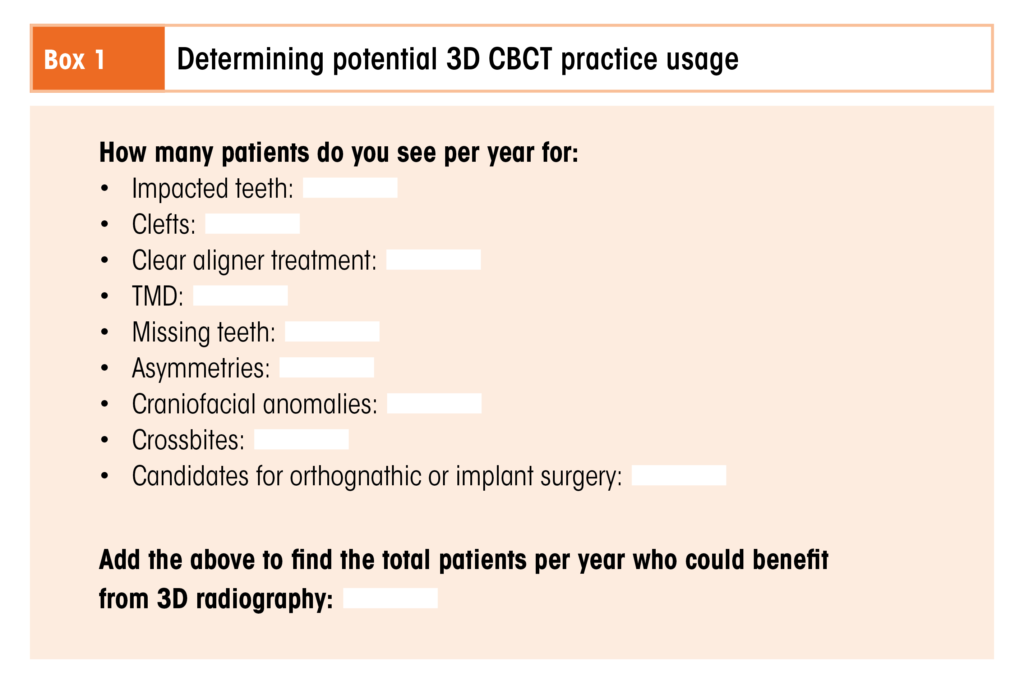
The first step in deciding whether you should purchase a 3D CBCT machine for your orthodontic practice is to determine how often you would use the machine. But what are specific clinical indications where 3D radiography is preferred over 2D?
“There are several indications common to the orthodontic practice where 3D CBCT should replace 2D radiographs as part of the initial diagnostic records collection or as soon as possible after a problem is suspected,” Dr Kula explains. “These indications include suspected dental agenesis or impactions, missing teeth, various temporomandibular disorder signs or symptoms, facial and dental asymmetries, craniofacial anomalies, and crossbites. 3D CBCTs are also indicated for patients who will potentially have orthognathic surgery or implant placement.”
“Patients with airway disorders and obstructive sleep apnea should also receive a 3D radiograph,” Dr Ghoneima adds.
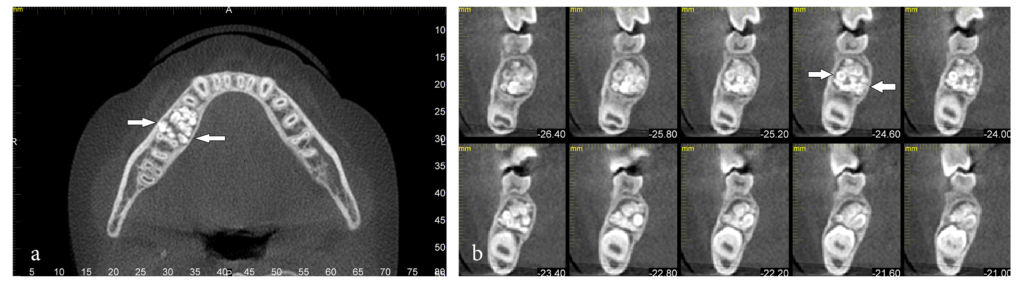
This compound odontoma (arrows) was discovered in an 11-year-old boy who was being evaluated for orthodontic treatment. (a) Axial view. (b) Cross-sectional views.
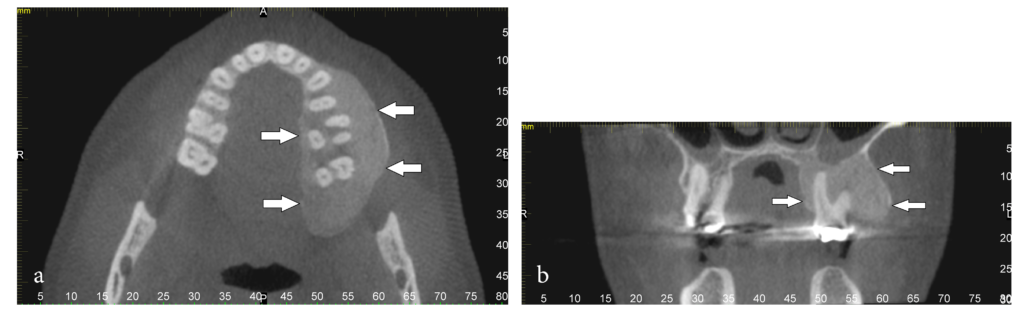
A 43-year-old man with fibrous dysplasia of the maxilla (arrows). The patient stated that his jaw began enlarging at 15 years of age. (a) Axial section of a CBCT scan through the maxilla. (b) Coronal view.
Eric Dellinger, DDS, MSD, breaks down his clinic’s 3D CBCT usage numbers in a chapter on cost comparison between 2D and 3D radiology in Cephalometry in Orthodontics: 2D and 3D: “The ability to refine diagnosis for patients with clefts, impacted canines, or craniofacial dysostosis might be a rarity in some offices. Within my own office, each year we see about 12 patients with clefts, 100 patients with impacted teeth, and 24 patients presenting for clear aligner treatment. Thus, we see only 136 patients per year who can potentially benefit from a 3D scan.”
Clinicians must consult their own numbers, as statistics from public data may be too general to be applicable. “Most research indicating the frequency of the types of patient anomalies that are indications for a 3D CBCT are usually based on the general population,” Dr Kula explains, “whereas these problems will naturally present more often in an orthodontic office than in the general population.”
Cost
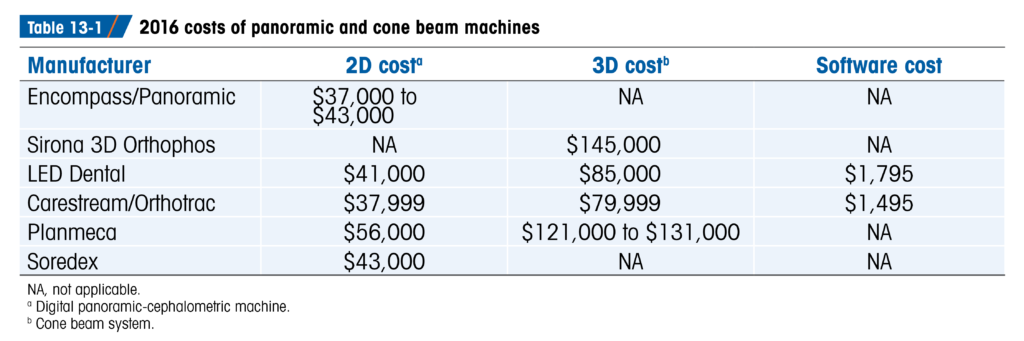
Once you’ve established the prospective amount of usage for your clinic, you can now perform a cost analysis to see just how feasible the purchase of a 3D CBCT machine is for your practice. There are two important factors to consider when thinking about the cost of a 3D CBCT machine: the first is the cost of the machine itself, and the second is the cost of a CBCT scan to your patients.
“In my review of costs, I found a $44,000 increase in cost for a 3D machine relative to a traditional panoramic-cephalometric machine,” Dr Dellinger states. “This is significantly reduced from the difference of $100,000 or more that was the norm a few years ago. Nonetheless, this cost is a twofold increase in the normal cost for digital x-ray equipment, and thus the expense must be covered by supplemental treatment fees.”
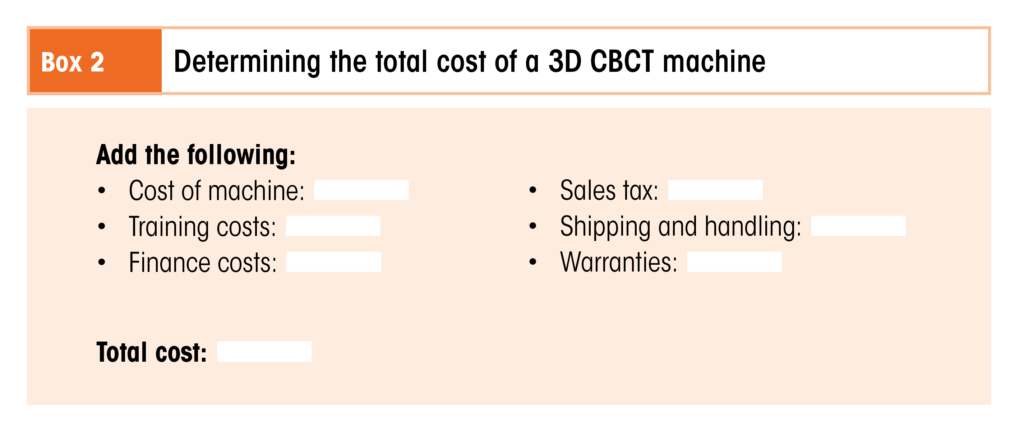
In addition to the sticker price of the machine, prospective buyers must also factor in additional costs like 3D software, warranties, and shipping and handling, as well as any applicable finance costs in order to calculate the full cost of implementing the technology into their practice. Staff members must receive training on the use of the machine, and the clinician or designated staff must also be trained on how to read and interpret the scans produced.
“With all of these extra charges,” Dr Dellinger says, “the final cost of the machine amortized over a 3-year period adds up to $2,000 for training (8 hours for 10 people) + $85,000 machine cost + finance costs of $6,711 (if the total of $85,000 is financed at 5% over 3 years) + $5,950 in sales tax (7% in Indiana) + $2,300 for shipping + $5,000 for warranties = $106,961. Thus, much like an automobile purchase, the total cost of the machine can be deceptively higher than the reduced sticker price may appear. As always, when approaching a significant expense for your practice, professional advice from your accountant may be very helpful in avoiding unpleasant surprises.”
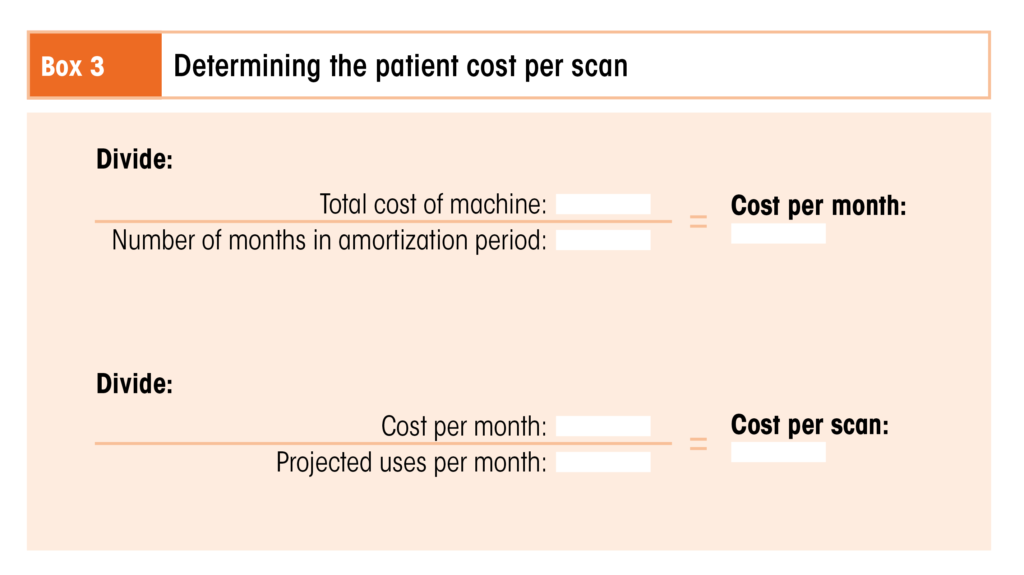
To determine the cost to your patients per scan, you can divide the total cost of the machine by the projected usage.
“If we assume a $100,000 cost divided over a 3-year amortization period,” Dr Dellinger calculates, “this comes to $2,778 per month. Assuming 20 uses per month, this leaves a cost of $138 per usage of the machine. By the same token, a 2D panoramic-cephalometric machine used 40 times per month at an initial cost of $45,000 (including some financing and training fees as well) comes to a price of only $62.50 per usage. Allowing these rough estimates, we see that the cost of 3D digital radiology will be about twice the cost of panoramic radiology. The choice of charging more for 3D scans and submitting this charge to medical insurance is also an option to defray costs. While the advantages of surgical evaluation of sinus structure and bone support can be invaluable in situations of cleft repair and impacted canines and third molars, and although this information is useful to orthodontists, the cost may exceed that of a referral to a radiology clinic for an MRI or 3D scan for evaluation of the patient, particularly in offices with fewer patients.”
Once you’ve done the numbers, one question remains: Is it worth it?
“Despite the additional monetary costs involved with 3D imaging, I find the personal reassurance of knowing the exact location of impactions and clefts to be of significant value,” Dr Dellinger emphasizes. “The confidence of knowing the precise positions of anatomy can lead to a much happier and confident clinician as well as a better treatment result for our patients. The cost of a 3D scan can thus produce several psychologic benefits, and these benefits can easily justify the additional cost for many clinicians. Given the advantages of 3D technology, it seems likely that we will continue to see improvements in this technology as well as increases in its use within dentistry and specifically within the practice of orthodontics.”
The Importance of Knowledge
Regardless of whether you decide to purchase a 3D CBCT machine for your own practice, it remains that we cannot go backward—only forward. We cannot ignore that there is now an option that can provide better, necessary information in many treatment circumstances. Clinicians must therefore prepare themselves to access and utilize this information through whatever means possible, whether by procuring their own 3D radiologic equipment or by referring their patients out for scans. Part of that preparation involves learning how to interpret the data produced in a 3D image using cephalometric principles.
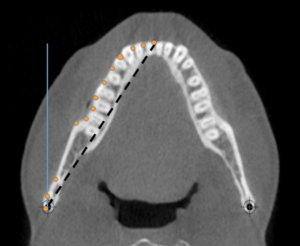
A 3D cone beam computed tomography (CBCT) section illustrating the differences in lengths if a 3D object is measured from one posterior lateral landmark to another anterior midline landmark from a 2D lateral perspective (blue line) or a 2D axial CBCT perspective (dashed black line). The actual length would be different if the perimeter of the object was measured (series of orange dots) because of the curve (3D CBCT perspective).
“Although not all clinicians will decide to include a 3D CBCT machine in their practice,” Dr Kula acknowledges, “they should be aware of the benefits that 3D radiology can provide to both the clinician and the patient. 3D radiology helps to optimize treatment outcomes and minimize risks such as the eruption of impacted teeth causing resorbed roots. Using 3D radiography, the clinician can ensure that patients are informed of the difficulty of their case and the reason for extra costs such as the extraction of impacted teeth. Clinicians who do not have a 3D CBCT machine in their office should be prepared to refer those patients to a clinic or imaging center that can provide a scan for pathology and a reading of the radiograph along with the image. In addition, the clinician should understand that 3D cephalometry is approximately a 1:1 image with minor magnification and that measurements from a 3D perspective are not always the same in a 2D measure, eg, profile or frontal.”
“Many clinicians,” Dr Ghoneima cautions, “may change their original treatment plan once they look at 3D images of their patients. This is because of hidden findings that could not be identified using conventional 2D images. For example, a patient may have significant root resorption due to ectopically impacted canines or a root fracture due to trauma. It is recommended that clinicians take a 3D radiograph if there is any uncertainty at all toward specific abnormal structures.”
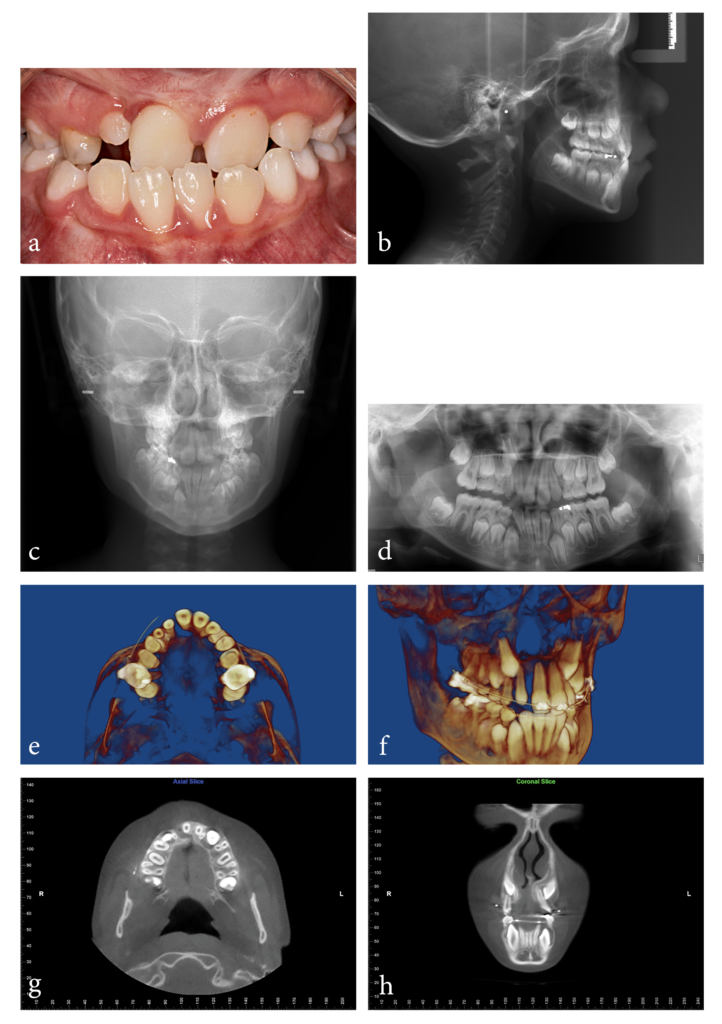
(a) Pretreatment intraoral photograph of a 9-year-old boy who was referred from the Cleft and Craniofacial Team with a diagnosis of cleft lip and no other significant medical history. Upon observing the thick frenum and a microdont maxillary lateral incisor, Dr Kula began to suspect there was an additional underlying issue. (b) Pretreatment lateral cephalogram. (c) Pretreatment frontal cephalogram. (d) Pretreatment panoramic radiograph. The panoramic radiograph showed probable impaction of the maxillary right canine and an indentation of the alveolar bone in the area between the microdont right lateral incisor and the right central incisor. The indentation appeared to continue toward the alveolar crest. At this point, the decision was made to take a 3D CBCT scan based on the appearance of the anterior maxillary arch, the frenum, nasal asymmetry, and the grooving observed in the panoramic radiograph. (e and f) Progress 3D CBCT reconstructions showing obvious clefting between the right central and lateral incisors from an axial view and a semilateral view. (g) Axial CBCT section showing the cleft with lack of alveolar continuity between the right lateral and central incisors. (h) Coronal CBCT section showing the position of the maxillary canines relative to the lateral incisor roots. The cleft was masked in the panoramic radiograph by two overlapping pieces of alveolar bone. The alveolar bone anterior to the maxillary and mandibular incisors was minimal. The alveolar bone palatal to the maxillary right central incisor was also minimal.
Information like that—information that can significantly influence a treatment plan—is invaluable to both the clinician and the patient. But in order to access it in full, clinicians must learn 3D cephalometric principles.
“The learning curve for 3D cephalometry is longer than for 2D cephalometry,” Dr Kula says. “For example, identification of a landmark from three perspectives—axial, coronal, and sagittal—takes a longer time. Landmark definitions are different because of the difference in perspective, and, unlike 2D cephalometry where landmark definitions are well established, landmark standards for 3D cephalometry still need to be developed and agreed upon. The learning curve for 3D cephalometry is shorter for clinicians who are introduced to it during residency programs compared with later, when practice management becomes a crucial focus for the orthodontist.”
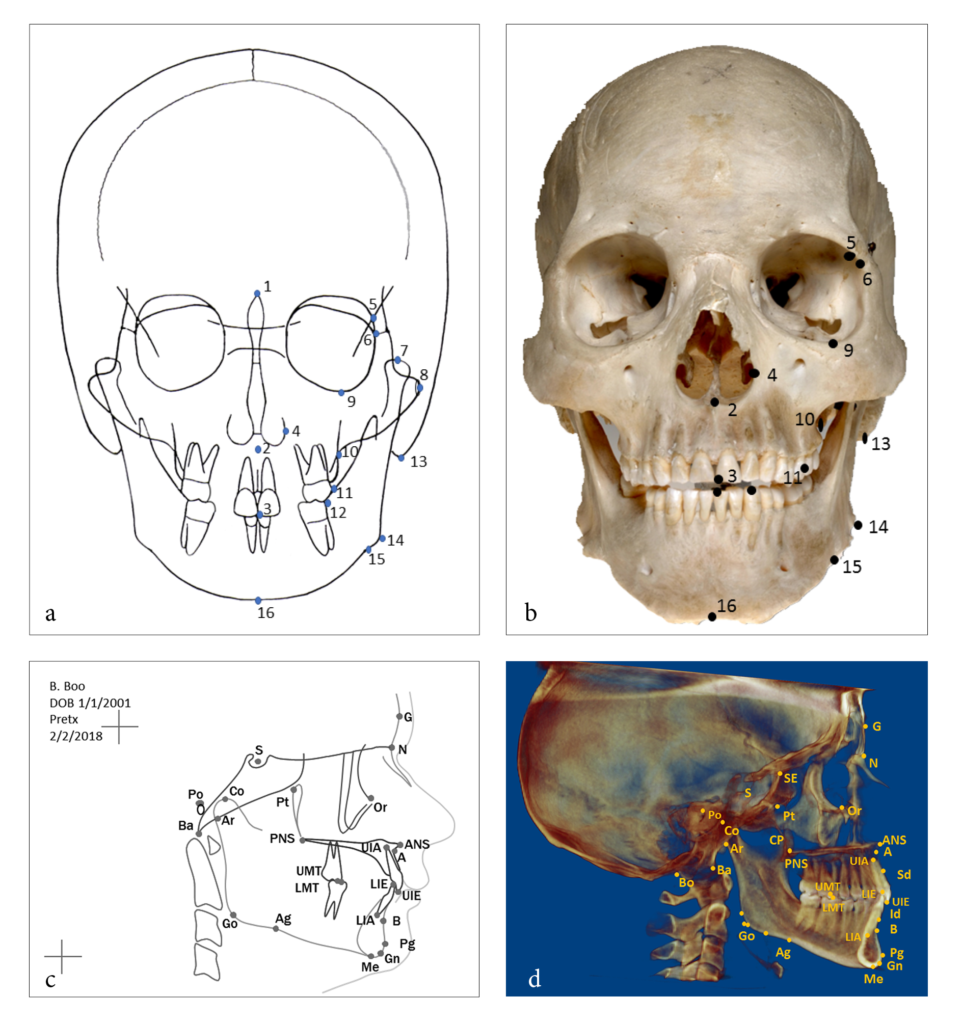
Note the differences between landmark locations on a 2D and 3D view and the addition of landmarks only visible using 3D CBCT. (a) Frontal landmarks on a manual tracing from a radiograph and (b) on a dry skull (only external landmarks can be marked). (c) 2D cephalometric tracing identifying (dots) and labeling (acronyms) landmarks. Labeling usually is not needed when the clinician is familiar with the landmarks. (d) Identification of landmarks on a 2D rendition of 3D CBCT.
There are several differences between the landmark locations on the 2D tracing compared with the 2D rendition of a 3D CBCT. One example is the gonion (Go), which is defined as the external angle of the mandible and located on the lateral radiograph by bisecting the angle formed by tangents to the posterior border of the ramus and the inferior border of the mandible (a line from menton to the posteroinferior border of the mandible).
“This learning curve gets easier to manage,” Dr Ghoneima adds, “once we have familiarized ourselves with this technology and how to manipulate the images to find the region of interest (ROI) in just a few clicks.”
It makes sense that as our technology changes, so must our knowledge base. Clinicians just starting to implement this technology must be aware that while 2D cephalometric principles may form the foundation of 3D cephalometry, the translation of knowledge is not one to one, and there is a great deal of new information to learn. Individual landmark definitions differ between 2D and 3D cephalometry, and there are important anatomical structures that can only be visualized using 3D imaging, leading to additional landmarks. And because landmark identification errors are considered a major source of cephalometric error, clinicians must obtain knowledge in 3D cephalometry that goes beyond understanding how to take a 3D CBCT scan.
The Future of 3D Cephalometry in Orthodontics
So will 2D radiology in orthodontics ever be completely replaced by 3D radiology, or will both continue to have unique benefits?
“Trying to answer that,” Dr Kula says, “reminds me of cartoons. The Flintstones makes me consider the wheel and how long it has been used. Despite numerous technological advances, the basic concept of the wheel still transports most of us. Several of the futuristic appliances from The Jetsons such as flat-screen televisions, video chatting, digital newspapers, and robotic vacuum cleaners have reached the common person, although others like flying cars, houses in the sky, and space tourism have not. It’s hard to predict what changes the near future will bring. But the answer of whether 3D radiology will replace 2D probably lies in patient need, ease of use, cost, radiation exposure, resolution, technological advancement, and marketing. As the technology improves, many of these variables are still changing, so only time will tell where it takes us.”
The space in time we occupy right now may feel closer to that of The Jetsons than The Flintstones, but every technological innovation we create is influenced by those that came before it. Likewise, 2D cephalometric knowledge forms the basis of 3D cephalometric knowledge. Cephalometry in Orthodontics: 2D and 3D creates a bridge between these two areas of knowledge so that clinicians can use both effectively, in turn enabling the clinician to practice 3D cephalometry no matter how they access the radiologic equipment.
 Katherine Kula, MS, DMD, MS, retired as Jarabak Endowed Professor and Chairperson for the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana. A board-certified orthodontist, Dr Kula taught and practiced for more than 40 years. She has authored more than 100 papers and 18 chapters, edited 4 books and monographs, and is the recipient of several national research awards and grants. In addition to her activities in professional societies, Dr Kula organized the first meeting involving the American Dental Association (ADA) and the US Food and Drug Administration regarding the approval of dental therapeutics and devices, and her research is cited in the ADA’s stance concerning the effect of acidulated phosphate fluorides on dental materials. Her research interests currently include three-dimensional imaging, technology, music, growth and development of the craniofacial complex, and forensic facial reconstruction.
Katherine Kula, MS, DMD, MS, retired as Jarabak Endowed Professor and Chairperson for the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana. A board-certified orthodontist, Dr Kula taught and practiced for more than 40 years. She has authored more than 100 papers and 18 chapters, edited 4 books and monographs, and is the recipient of several national research awards and grants. In addition to her activities in professional societies, Dr Kula organized the first meeting involving the American Dental Association (ADA) and the US Food and Drug Administration regarding the approval of dental therapeutics and devices, and her research is cited in the ADA’s stance concerning the effect of acidulated phosphate fluorides on dental materials. Her research interests currently include three-dimensional imaging, technology, music, growth and development of the craniofacial complex, and forensic facial reconstruction.
 Ahmed Ghoneima, BDS, PhD, MSD, is Associate Professor of Orthodontics and Graduate Program Director of the College of Dental Medicine at Mohammed Bin Rashid University of Medicine and Health Sciences in Dubai, United Arab Emirates. He received his dental degree and master of science from Al-Azhar University in Cairo, Egypt, and his PhD from the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana, where he became a full-time faculty member. His research program focuses on airway analysis, applications of three-dimensional imaging in orthodontics, haptic technology, and the use of virtual reality in dental education. Dr Ghoneima is the recipient of numerous prestigious awards, including the Michael Matlof Memorial Teaching Fellowship Award and the Orhan C. Tuncay Teaching Fellowship Award, both from the American Association of Orthodontists Foundation, as well as the Academy for Academic Leadership Award. He has previously chaired the Indiana Section of the American Association for Dental Research and currently holds the position of Chair Elect for the American Dental Education Association section on orthodontics. He also serves as a reviewer for several peer-reviewed orthodontic journals.
Ahmed Ghoneima, BDS, PhD, MSD, is Associate Professor of Orthodontics and Graduate Program Director of the College of Dental Medicine at Mohammed Bin Rashid University of Medicine and Health Sciences in Dubai, United Arab Emirates. He received his dental degree and master of science from Al-Azhar University in Cairo, Egypt, and his PhD from the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana, where he became a full-time faculty member. His research program focuses on airway analysis, applications of three-dimensional imaging in orthodontics, haptic technology, and the use of virtual reality in dental education. Dr Ghoneima is the recipient of numerous prestigious awards, including the Michael Matlof Memorial Teaching Fellowship Award and the Orhan C. Tuncay Teaching Fellowship Award, both from the American Association of Orthodontists Foundation, as well as the Academy for Academic Leadership Award. He has previously chaired the Indiana Section of the American Association for Dental Research and currently holds the position of Chair Elect for the American Dental Education Association section on orthodontics. He also serves as a reviewer for several peer-reviewed orthodontic journals.
 Cephalometry in Orthodontics: 2D and 3D
Cephalometry in Orthodontics: 2D and 3D
Edited by Katherine Kula and Ahmed Ghoneima
Cephalometrics has been used for decades to diagnose orthodontic problems and evaluate treatment. However, the shift from 2D to 3D radiography has left some orthodontists unsure about how to use this method effectively. This book defines and depicts all cephalometric landmarks on a skull or spine in both 2D and 3D and then identifies them on radiographs. Each major cephalometric analysis is described in detail, and the linear or angular measures are shown pictorially for better understanding. Because many orthodontists pick specific measures from various cephalometric analyses to formulate their own analysis, these measures are organized relative to the skeletal or dental structure and then compared or contrasted relative to diagnosis, growth, and treatment. Cephalometric norms (eg, age, sex, ethnicity) are also discussed relative to treatment and esthetics. The final chapter shows the application of these measures to clinical cases to teach clinicians and students how to use them effectively. As radiology transitions from 2D to 3D, it is important to evaluate the efficacy and cost-effectiveness of each in diagnosis and treatment, and this book outlines all of the relevant concerns for daily practice.
208 pp; 338 illus; ©2018; ISBN 978-0-86715-762-8 (B7628); US $118

Pingback: Quintessence Roundup: October | Quintessence Publishing Blog
Pingback: Quintessence Roundup: November | Quintessence Publishing Blog