 Implant dentistry has evolved significantly since Per-Ingvar Brånemark first introduced the idea of osseointegration to North America in the 1980s. This paradigm shift in treatment purpose has led to a transition from primarily integration and survival goals to prioritizing biologic and esthetic goals.
Implant dentistry has evolved significantly since Per-Ingvar Brånemark first introduced the idea of osseointegration to North America in the 1980s. This paradigm shift in treatment purpose has led to a transition from primarily integration and survival goals to prioritizing biologic and esthetic goals.
Enter Dennis P. Tarnow, DDS, and Stephen J. Chu, DMD, MSD, CDT, who have worked for three decades as clinicians, instructors, and researchers in domestic and international continuing dental education. The relationship of this world-renowned surgeon and world-renowned prosthodontist duo working hand-in-hand has been an asset to their practice.
“It is difficult to be an expert in both surgery and prosthetics since there is so much to learn and know,” Dr Chu explains. “The best part of working in the same environment is that we can treat the patient without that individual having to run to different offices to accomplish the same goal.”
“When both clinicians are together, the treatment transition from surgery to prosthodontics is seamless.”
Their close collaboration of 15 years has also resulted in a sense of appreciation for each specialist’s abilities, directly translating to better patient care.
“The communication and understanding of what must be done for the patient is crystal clear,” Dr Chu says. “Oftentimes when clinicians are physically in separate offices, communication in treatment can be muted. When both clinicians are together, the treatment transition from surgery to prosthodontics is seamless.”
The most recent collaboration of Drs Tarnow and Chu resulted in The Single-Tooth Implant: A Minimally Invasive Approach for Anterior and Posterior Extraction Sockets. Written by clinicians for clinicians, this textbook capitalizes on the idea of “one surgery, one time” and progresses from simple to complex single-tooth implant scenarios.
Immediate Tooth Replacement Therapy
Replacement of a single tooth with a dental implant is one of the most common situations clinicians encounter on a daily basis. In fact, it makes up about half of daily implant cases, many of which occur in the esthetic zone.
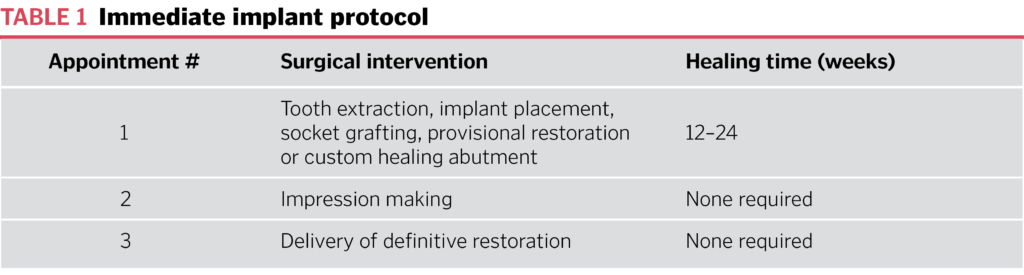
Immediate tooth replacement therapy yields survival rates equal to, if not higher than, delayed implant placement. Delayed placement allows for soft tissue maturation and site development prior to placement, but this advantage occurs at the expense of increased treatment time.
On the other hand, immediate placement allows for decreased treatment time, fewer appointments, and higher patient comfort. Most importantly, it makes preservation of the natural architecture of surrounding hard and soft tissues possible at the time of tooth removal, which is a distinct advantage in today’s esthetics-focused culture. This is in line with the ultimate goal of therapy: to preserve, maintain, and protect existing tissues, rather than introducing the opportunity for esthetic error by attempting to recreate lost tissue.
This predictable restorative and esthetic outcome is possible with proper 3D implant placement, platform switching, and soft tissue support with a provisional restoration. However, immediate replacement has its own challenges, the most common being a collapse of the facial ridge with midfacial recession, resulting in integration success but esthetic failure due to loss of the labial bone plate. While immediate tooth replacement therapy is an excellent choice for many cases, it is not ideal for every situation because not all extraction sockets are alike.
 Inverted Implant Technique
Inverted Implant Technique
It is well known that the labial bone plate and soft tissues in the anterior maxilla are at risk of esthetic dilemmas due to their extremely thin diameter (1 mm or less). Preventing greater than 1 mm of tissue collapse—the threshold for esthetic success—is ideal. While wide implants are most effective at achieving stability, narrow implants should still be considered. Altering the implant length is another possibility, but diameter is more effective at achieving stability than length. However, the wider-diameter, tapered implant design is a poor choice.
It is possible to mitigate the width/length dilemma and achieve the “best of both worlds” with a new, unique “body-shift” concept, or “inverted” body implant design.
Even with the modern switch from an implant survival to an esthetic results mindset, it is possible to mitigate the width/length dilemma and achieve the “best of both worlds” with a new, unique “body-shift” concept, or “inverted” body implant design. This innovative, macro hybrid design combines a tapered apical portion with a cylindrical coronal portion, all in a single body.
“The inverted body-shift concept uses the strategy of changing the diameter and shape of the implant in a singular design,” Dr Chu says. “It’s a happy medium: the primary stability of a larger-diameter implant (apically) and the size of a smaller implant where the bone is thinnest (coronally). More graft material can be placed in this coronal chamber, which increases the thickness around the implant. Also, by reducing the top, the distance between the tooth and the implant is increased to preserve the papilla.”

(a and b) The inverta implant design combines a tapered apical portion with a cylindrical coronal portion, all in a singular body. (c and d) Greater space is inherently generated that allows more graft material to be placed, not only labially but also interdentally into the gap, to create a net increased bone dimension.
Ice Cream Cone Technique
The Single-Tooth Implant: A Minimally Invasive Approach for Anterior and Posterior Extraction Sockets walks the reader through three types of extraction sockets. Type 2 occurs when soft tissues remain intact but the labial bone plate possesses a dentoalveolar dehiscence defect, which increases the risk of midfacial recession.
Fortunately, a solution has been developed: a socket repair procedure called the ice cream cone technique, which allows for reconstruction of the buccal plate dehiscence to enable implant placement.
This technique derives its name from the shape of the absorbable cross-linked collagen membrane, which is contoured into a modified V-shape, or ice cream cone shape. This membrane is placed into the socket cone-side first, and the ice cream side is trimmed to cover the socket opening after graft placement. The membrane lines the socket’s buccal tissues while the socket is filled with bone graft material that is compressed into the socket. The pressure of the graft against the buccal tissue holds the membrane in place. Finally, the membrane is sutured to the palatal tissue, covering the socket.

(a) Type 2 socket with intact soft tissue but a midfacial osseous dehiscence defect. (b) Atraumatic tooth extraction without flap elevation. (c) Socket after tooth extraction and debridement. (d) Collagen membrane contoured into a modified V or ice cream cone shape. (e) Placement of the ice cream cone collagen membrane. (f) Socket filled with graft material. (g) The membrane is extended over the socket and sutured. (h and i) Socket after absorption of the collagen membrane and graft incorporation.
“The ice cream cone technique is a simplified way to combine socket preservation of an extraction socket while being able to build back the missing buccal plate of bone at the same time,” Dr Tarnow explains. “This is all done with a minimally invasive procedure that requires no flap. The membrane, which must be made of a collagen that maintains its rigidity after getting wet, is the key to success. The part that is placed into the socket (the cone part) prevents the soft tissue on the buccal side of the socket from migrating into the graft material before the bone does so. It is guided bone regeneration.”
“The ice cream cone technique is a simplified way to combine socket preservation of an extraction socket while being able to build back the missing buccal plate of bone at the same time.”
The authors recommend using a graft material that is a small-particle, mineralized cancellous freeze-dried bone allograft because it compresses well, maintains shape, and resorbs slowly.
“The ice cream part placed over the top of the socket will only last for a couple of weeks,” Dr Tarnow says, “but it is enough time to contain the graft particles and protect the clot during the first phase of healing.”
The Single-Tooth Implant: A Minimally Invasive Approach for Anterior and Posterior Extraction Sockets covers both the inverted implant and ice cream cone techniques in depth, and more.
“This is my fourth time working with Quintessence,” Dr Chu recalls. “It’s about conveying concepts to the next generation, which is our legacy. The book is outlined and constructed in such a way as to teach concepts from more simple to complex case types for single-implant therapy with minimally invasive techniques for both anterior and posterior sites.”
To learn more about Dr Chu’s previous book, Color in Dentistry: A Clinical Guide to Predictable Esthetics, check out our article Current Challenges in Color.
 Dennis P. Tarnow, DDS, is a clinical professor of periodontology and director of implant education at Columbia School of Dental Medicine. He is a recipient of the Master Clinician Award from the American Academy of Periodontology, Teacher of the Year Award from NYU, and Distinguished Lecturer Award from the American College of Prosthodontists. He has published over 150 articles on perio-prosthodontics and implant dentistry and has coauthored three textbooks, including Aesthetic Restorative Dentistry: Principles and Practice (Montage Media, 2008). Dr Tarnow maintains a private practice in New York City and has lectured in over 30 countries, including the United States.
Dennis P. Tarnow, DDS, is a clinical professor of periodontology and director of implant education at Columbia School of Dental Medicine. He is a recipient of the Master Clinician Award from the American Academy of Periodontology, Teacher of the Year Award from NYU, and Distinguished Lecturer Award from the American College of Prosthodontists. He has published over 150 articles on perio-prosthodontics and implant dentistry and has coauthored three textbooks, including Aesthetic Restorative Dentistry: Principles and Practice (Montage Media, 2008). Dr Tarnow maintains a private practice in New York City and has lectured in over 30 countries, including the United States.
 Stephen J. Chu, DMD, MSD, CDT, is an associate clinical professor in the Ashman Department of Periodontology and Implant Dentistry and the Department of Prosthodontics as well as the director of esthetic education at the New York University College of Dentistry. He has published more than 40 articles and given lectures nationally and internationally on the subjects of esthetic, restorative, and implant dentistry. Dr Chu is a coauthor of the book Color in Dentistry: A Clinical Guide to Predictable Esthetics (Quintessence, 2017) and is on the editorial review board of several peer-reviewed dental journals. He is the recipient of the Peter Scharer Distinguished Lecturer Award from the European Academy of Esthetic Dentistry and the Lloyd L. Miller Distinguished Lecturer Award from the Society for Color and Appearance in Dentistry. Dr Chu maintains a private practice limited to fixed prosthodontics, esthetic dentistry, and implant dentistry in New York City.
Stephen J. Chu, DMD, MSD, CDT, is an associate clinical professor in the Ashman Department of Periodontology and Implant Dentistry and the Department of Prosthodontics as well as the director of esthetic education at the New York University College of Dentistry. He has published more than 40 articles and given lectures nationally and internationally on the subjects of esthetic, restorative, and implant dentistry. Dr Chu is a coauthor of the book Color in Dentistry: A Clinical Guide to Predictable Esthetics (Quintessence, 2017) and is on the editorial review board of several peer-reviewed dental journals. He is the recipient of the Peter Scharer Distinguished Lecturer Award from the European Academy of Esthetic Dentistry and the Lloyd L. Miller Distinguished Lecturer Award from the Society for Color and Appearance in Dentistry. Dr Chu maintains a private practice limited to fixed prosthodontics, esthetic dentistry, and implant dentistry in New York City.
 The Single-Tooth Implant: A Minimally Invasive Approach for Anterior and Posterior Extraction Sockets
The Single-Tooth Implant: A Minimally Invasive Approach for Anterior and Posterior Extraction Sockets
Dennis P. Tarnow and Stephen J. Chu
The replacement of the single tooth with a dental implant is one of the most common clinical situations practitioners face on a daily basis. While in the past sockets were left untouched for months after tooth extraction before attending to the residual ridge, today it is possible to perform “one surgery, one time,” which is a huge benefit to both the patient and clinician alike. Written by two world-class masters, this book begins with a discussion of the history and rationale for anterior and posterior single-tooth implants, and then it walks the reader through the three types of sockets—type 1, type 2, and type 3—and their various indications and limitations. An entire chapter is devoted to clinical management of posterior teeth, followed by a chapter on cementation and impression-making techniques and complications. The final chapter is a clinical case appendix detailing 11 cases of single-tooth replacement in all types of sockets previously described. The protocols showcased in this book will make patient care faster, easier, simpler, more predictable, and, in many cases, less costly.
240 pp; 1,117 illus; ©2020; ISBN 978-0-86715-771-0 (B7710); US $228
Contents
1. History and Rationale for Anterior and Posterior Single-Tooth Implants
2. Management of Type 1 Extraction Sockets
3. Management of Type 2 Extraction Sockets
4. Management of Type 3 Extraction Sockets
5. Clinical Management of Posterior Teeth
6. Important Considerations in Implant Dentistry
7. Clinical Case Appendix
This article was written by Sarah Mondello, Quintessence Publishing.
©2019 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
