Reading time: 8 minutesFor several years, dentistry has been in a period of transition and innovation, as technologic developments outpace our ability to implement them. In the fields of implants and prosthetics, digital advances have completely transformed the way we plan cases—it is now possible to plan a case entirely virtually.
So should we immediately forget about the old methods and fully embrace this new technology? Stop teaching analog dentistry to our students and younger colleagues because they’ll never need to use it? Not so fast. While digital dentistry may be the future, it is not foolproof, and a fundamental understanding of the analog concepts behind it is required to have predictable success with this type of treatment. This was the reasoning behind the latest book from Drs Bedrossian, Bedrossian, and Brecht, a clinical text focused on immediate implants that explores cases from a 2D and 3D point of view to ensure the greatest success. As Edmond Bedrossian explains, “the digital workflow is powered by fundamental analog principles.”

Ways to Incorporate a Digital Workflow
Using a digital workflow is not an all-or-nothing concept. The 3D scan can be imported into the planning software for a comprehensive view of the patient’s anatomy, and the case can be completed traditionally from there on. Or, the clinician can pick and choose a combination of analog and digital workflow steps for planning and execution of implant therapy.
Digital workflows can be used for the planning phase of treatment, the surgical phase of treatment, and the restorative/laboratory phase of treatment, as follows:
- Planning phase
- Planning implant positions
- Planning abutment type and angle
- Optimizing implant angulation
- Surgical phase
- Printing an anatomical model for practice surgery
- Printing surgical guides and stents
- Printing a provisional prosthesis
- Restorative/laboratory phase
- Printing study models
- Taking an intraoral scan of the implant positions instead of impressions
- Communication with the dental technician in designing the prosthesis
- Generating prototype PMMA models to evaluate the esthetic and functional needs of the patient
- Fabrication of the definitive prosthesis

Virtual implant planning.
Advantages of a Digital Approach
One huge advantage of the digital workflow is ease of communication. First, communication can occur more quickly by sending digital files among clinicians and laboratory technicians in an instant. Communication is also improved with the patient, as they can view the 3D models and planning steps on the screen throughout the treatment planning process.

Virtual restoration planning.
Additional advantages of a complete digital workflow protocol include saving of chair time, reduction of cost, optimization of clinical prosthodontic procedures through use of digital workflow, and improvement of patient satisfaction with reduction of treatment time.
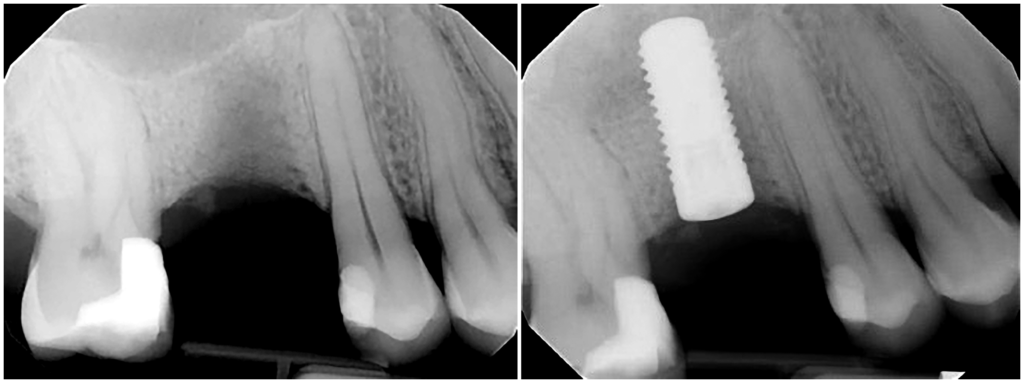
With 3D scanning, you can virtually plan an entire case before you actually do it, foreseeing problems and learning what may or may not work. This allows a perfect path to be created for the implant, avoiding anatomical features that have been identified with a CBCT scan and ensuring enough space will remain around the implant in all three dimensions. To reflect this perfect path, a surgical guide can be printed to be used in surgery.
In spite of this, having knowledge and experience in analog surgical planning and placement is necessary, allowing the clinician to better understand when and how to manipulate bone to optimize primary implant stability and to be able to navigate and manage intrasurgical challenges or complications. Expertise and experience cannot be replaced with guided surgery.
In addition, procedures such as bone and soft tissue grafting still require a mix of virtual and analog methods. Anticipating the extent of the tissue management requirements and challenges of treatment before surgery is of immense value, but the procedures themselves are largely analog.
Steps Required for Digital Workflow

First, the data must be gathered with a CBCT scan and intraoral scan. This will result in a DICOM file and STL file which are brought together to plan the case. The data sets must be imported into a software program, segmented, and accurately aligned, either using built-in algorithms for best matching, or at times marked and merged by the planning team member. This is the most important preparatory step, since the interaction between hard and soft tissue structures will drive the prosthetically planned implant positioning and tissue management strategies.

Joining of DICOM and STL files.
Perhaps the greatest challenge lies in the capture of soft tissue emergence profiles when the tissue phenotype is thin and less stable or when an implant is deeply positioned in tissue and bone and difficult to scan the prosthetic tissue envelope. It is important to remember that it is absolutely acceptable to introduce analog steps like standard impressioning if necessary. Tissue scanning challenges can be managed by scanning or impressing the provisional restoration outside of the mouth to record the emergence profile if it is satisfactory.

IOS, intraoral scanning.
Challenges also emerge when scanning fully edentulous arches. The absence of anatomical landmarks such as teeth within the data acquisition procedures and intraoral scanning represents a challenge for the registration and data superimposition. Because of the absence of solid anatomical landmarks, the merging, registration, and virtual articulation of the STL files that are generated from the digital scan of the implant scan bodies and the screw-retained provisional prosthesis is not feasible. Although innovations are constantly emerging to overcome challenges such as these, there will be times when the best way forward will be to take a step back and reevaluate the case from another perspective.
Conclusion
Dr E. Armand Bedrossian may have said it best: “Digital technology has made it a very fun and exciting time to be in dentistry, and it’s hard to not come across a journal or symposium without a topic on how these technologies can and should be implemented in the dental practice. What I believe is shared amongst most clinicians, however, is the importance of a solid understanding of fundamental analog principles. Digital technology, whether it is being used for treatment planning by way of digital smile designs, computer-aided design for implant planning, or computer-aided manufacturing for additive 3D printing or subtractive milling, all require a foundation of analog principles allowing the clinician to utilize these contemporary techniques in an efficient and predictable manner. As I approach my fifth year in private practice, my daily treatment workflows have transitioned from alginate impressions and analog cross mounting, to now intraoral scanning and printing models to treatment plan the case. Being blessed with the opportunity to have such technologies in my practice have allowed me to provide comprehensive care for my patients in a modern yet efficient manner.”
As Dr Edmond Bedrossian adds, digital technology does not substitute the need for the implant team to have command of the analog principles whether from the surgical, restorative, or the laboratory perspective. Instead, the digital workflow is an elegant and efficient way to plan, communicate, and execute the various steps for treating patients in need of dental implants for rehabilitation of their oral health.
Learn more about the analog to digital workflow, in particular how it applies to immediate implants, in the forthcoming book The Immediacy Concept from Drs Bedrossian, Bedrossian, and Brecht.
 The Immediacy Concept: Treatment Planning from Analog to Digital
The Immediacy Concept: Treatment Planning from Analog to Digital
Edited by Edmond Bedrossian, E. Armand Bedrossian, and Lawrence E. Brecht
Immediate loading meets digital treatment planning in this latest implant title. The authors emphasize that the preservation of alveolar hard and soft tissues using the immediacy concept is more predictable than is the reconstruction of the hard and soft tissues using the traditional delayed approach once resorption has occurred. Immediate loading has also shown to be very predictable in cases of full-arch reconstructions and has become the treatment of choice in cases where appropriate criteria are met. Because a thorough understanding of analog protocols is necessary before attempting a digital case, the authors review these fundamental concepts to provide context for the transition to the digital realm. The book begins by outlining the principles of immediate loading and those of digital workflows before delving into individual clinical situations ranging from single teeth to full arches, both with and without bone resorption. Information on prosthetics is included as well as surgical treatment planning. The book concludes with a chapter entirely devoted to case presentations of all the treatment types covered throughout. If you are ready to step into the future of dental implant treatment, this book is for you!
408 pp; 1,153 illus; ©2022; 978-1-64724-042-4 (B0424)
Editors:
 Edmond Bedrossian, DDS, received his dental degree from the University of the Pacific, and completed his oral and maxillofacial residency at Alameda Medical Center. He is a professor in the department of oral and maxillofacial surgery at the University of the Pacific School of Dentistry, as well as the former director of implant surgery at Alameda County Oral & Maxillofacial Surgery training program. Dr Bedrossian has authored multiple articles and chapters as well as two books on the various uses of dental implants including bone grafting, immediate implant placement, and treatment of the fully edentulous patient with tilted as well as zygomatic implants. He serves on review boards for multiple peer-reviewed journals and is a diplomate of the American Board of Oral and Maxillofacial Surgery and an honorary member of the American College of Prosthodontists. Dr Bedrossian maintains a private practice limited to implant and oral and maxillofacial surgery in San Francisco, California.
Edmond Bedrossian, DDS, received his dental degree from the University of the Pacific, and completed his oral and maxillofacial residency at Alameda Medical Center. He is a professor in the department of oral and maxillofacial surgery at the University of the Pacific School of Dentistry, as well as the former director of implant surgery at Alameda County Oral & Maxillofacial Surgery training program. Dr Bedrossian has authored multiple articles and chapters as well as two books on the various uses of dental implants including bone grafting, immediate implant placement, and treatment of the fully edentulous patient with tilted as well as zygomatic implants. He serves on review boards for multiple peer-reviewed journals and is a diplomate of the American Board of Oral and Maxillofacial Surgery and an honorary member of the American College of Prosthodontists. Dr Bedrossian maintains a private practice limited to implant and oral and maxillofacial surgery in San Francisco, California.
 Edmond Armand Bedrossian, DDS, MSD, is a board-certified prosthodontist and currently practices in his hometown of San Francisco, California. He received his DDS from the University of the Pacific Arthur A. Dugoni School of Dentistry in 2015 and completed the advanced prosthodontics residency program and received his master’s degree at the University of Washington, where he is currently an affiliate assistant professor. He is a diplomate of the American Board of Prosthodontics and has authored various publications on removable prosthodontics and treatment planning the fully edentulous patient. He has lectured nationally and internationally on implant and prosthetic dentistry. Along with Dr Ryan Mizumoto, he co-founded D365, a social media application providing a networking platform for dental students, residents, and dental practitioners.
Edmond Armand Bedrossian, DDS, MSD, is a board-certified prosthodontist and currently practices in his hometown of San Francisco, California. He received his DDS from the University of the Pacific Arthur A. Dugoni School of Dentistry in 2015 and completed the advanced prosthodontics residency program and received his master’s degree at the University of Washington, where he is currently an affiliate assistant professor. He is a diplomate of the American Board of Prosthodontics and has authored various publications on removable prosthodontics and treatment planning the fully edentulous patient. He has lectured nationally and internationally on implant and prosthetic dentistry. Along with Dr Ryan Mizumoto, he co-founded D365, a social media application providing a networking platform for dental students, residents, and dental practitioners.
 Lawrence E. Brecht, DDS, received his dental degree from New York University College of Dentistry and completed his prosthodontics and maxillofacial prosthetics residencies at the Veterans Administration Medical Center in Manhattan. Dr Brecht is currently the director of maxillofacial prosthetics at Lenox Hill Hospital, Long Island Jewish Medical Center, and North Shore University Hospital of Northwell Health, the largest hospital system in New York State. In addition, he serves as the director of maxillofacial prosthetics in the postgraduate prosthodontics program of NYU College of Dentistry, where he is an adjunct associate clinical professor of prosthodontics. Dr Brecht has authored multiple articles and chapters on the maxillofacial reconstruction and oral rehabilitation of patients with cancer or craniofacial anomalies and is on the editorial review boards of several well-regarded journals. He serves as the president of the Maxillofacial Foundation as well as NextGenFace Foundation. Dr Brecht currently maintains a private practice limited to prosthodontics in New York City.
Lawrence E. Brecht, DDS, received his dental degree from New York University College of Dentistry and completed his prosthodontics and maxillofacial prosthetics residencies at the Veterans Administration Medical Center in Manhattan. Dr Brecht is currently the director of maxillofacial prosthetics at Lenox Hill Hospital, Long Island Jewish Medical Center, and North Shore University Hospital of Northwell Health, the largest hospital system in New York State. In addition, he serves as the director of maxillofacial prosthetics in the postgraduate prosthodontics program of NYU College of Dentistry, where he is an adjunct associate clinical professor of prosthodontics. Dr Brecht has authored multiple articles and chapters on the maxillofacial reconstruction and oral rehabilitation of patients with cancer or craniofacial anomalies and is on the editorial review boards of several well-regarded journals. He serves as the president of the Maxillofacial Foundation as well as NextGenFace Foundation. Dr Brecht currently maintains a private practice limited to prosthodontics in New York City.




 Dr Leandro Chambrone received a DDS and a Certificate in Orthodontics and Dentofacial Orthopedics from Methodist University of São Paulo in Brazil. Subsequently, he earned a master’s degree and PhD degree in periodontics from the University of São Paulo. He serves as a faculty member in several prestigious institutions in North America, South America, and Europe. He holds positions of Associate Professor at Egas Moniz University (Portugal), Ad honorem Associate Professor at El Bosque University (Colombia), Visiting Professor at the University of Iowa, and Adjunct Associate Professor at Penn School of Dental Medicine. Beyond his enthusiasm and dedication as an educator and health care provider, Dr Chambrone is also heavily involved in clinical research and evidence-based dentistry. He has authored over 150 papers, including some commissioned consensus reviews for the American Academy of Periodontology and the European Federation of Periodontology. Dr Chambrone currently serves as Section Editor of Clinical Research for The International Journal of Oral Implantology and Section Editor of Periodontics for the Journal of Esthetic and Restorative Dentistry.
Dr Leandro Chambrone received a DDS and a Certificate in Orthodontics and Dentofacial Orthopedics from Methodist University of São Paulo in Brazil. Subsequently, he earned a master’s degree and PhD degree in periodontics from the University of São Paulo. He serves as a faculty member in several prestigious institutions in North America, South America, and Europe. He holds positions of Associate Professor at Egas Moniz University (Portugal), Ad honorem Associate Professor at El Bosque University (Colombia), Visiting Professor at the University of Iowa, and Adjunct Associate Professor at Penn School of Dental Medicine. Beyond his enthusiasm and dedication as an educator and health care provider, Dr Chambrone is also heavily involved in clinical research and evidence-based dentistry. He has authored over 150 papers, including some commissioned consensus reviews for the American Academy of Periodontology and the European Federation of Periodontology. Dr Chambrone currently serves as Section Editor of Clinical Research for The International Journal of Oral Implantology and Section Editor of Periodontics for the Journal of Esthetic and Restorative Dentistry. Dr Gustavo Avila Ortiz obtained a DDS degree and completed his PhD at the University of Granada (Spain) before moving to Ann Arbor, Michigan, where he completed an MS degree and a Certificate in Periodontics at the University of Michigan. He has over 10 years of experience as an educator and has worked to advance the profession as a member of numerous institutional committees and scientific organizations; he is also a Diplomate of the American Board of Periodontology. He was a faculty member at the University of Michigan School of Dentistry and at the University of Iowa College of Dentistry, where he was the Phillip A. Lainson Professor and Chair of the Department of Periodontics. Dr Avila Ortiz serves as Associate Editor for the Journal of Periodontology and Co-Editor for Clinical Advances in Periodontics, the official journals of the American Academy of Periodontology. He has authored more than 100 articles published in peer-reviewed journals as well as several book chapters. Aside from being regularly engaged in scholarly, administrative, and continuing education activities in different academic institutions, Dr Avila Ortiz maintains a private practice limited to periodontics and implant dentistry at Atelier Dental in Madrid, Spain.
Dr Gustavo Avila Ortiz obtained a DDS degree and completed his PhD at the University of Granada (Spain) before moving to Ann Arbor, Michigan, where he completed an MS degree and a Certificate in Periodontics at the University of Michigan. He has over 10 years of experience as an educator and has worked to advance the profession as a member of numerous institutional committees and scientific organizations; he is also a Diplomate of the American Board of Periodontology. He was a faculty member at the University of Michigan School of Dentistry and at the University of Iowa College of Dentistry, where he was the Phillip A. Lainson Professor and Chair of the Department of Periodontics. Dr Avila Ortiz serves as Associate Editor for the Journal of Periodontology and Co-Editor for Clinical Advances in Periodontics, the official journals of the American Academy of Periodontology. He has authored more than 100 articles published in peer-reviewed journals as well as several book chapters. Aside from being regularly engaged in scholarly, administrative, and continuing education activities in different academic institutions, Dr Avila Ortiz maintains a private practice limited to periodontics and implant dentistry at Atelier Dental in Madrid, Spain.






 Edmond Bedrossian, DDS, received his dental degree from the University of the Pacific, and completed his oral and maxillofacial residency at Alameda Medical Center. He is a professor in the department of oral and maxillofacial surgery at the University of the Pacific School of Dentistry, as well as the former director of implant surgery at Alameda County Oral & Maxillofacial Surgery training program. Dr Bedrossian has authored multiple articles and chapters as well as two books on the various uses of dental implants including bone grafting, immediate implant placement, and treatment of the fully edentulous patient with tilted as well as zygomatic implants. He serves on review boards for multiple peer-reviewed journals and is a diplomate of the American Board of Oral and Maxillofacial Surgery and an honorary member of the American College of Prosthodontists. Dr Bedrossian maintains a private practice limited to implant and oral and maxillofacial surgery in San Francisco, California.
Edmond Bedrossian, DDS, received his dental degree from the University of the Pacific, and completed his oral and maxillofacial residency at Alameda Medical Center. He is a professor in the department of oral and maxillofacial surgery at the University of the Pacific School of Dentistry, as well as the former director of implant surgery at Alameda County Oral & Maxillofacial Surgery training program. Dr Bedrossian has authored multiple articles and chapters as well as two books on the various uses of dental implants including bone grafting, immediate implant placement, and treatment of the fully edentulous patient with tilted as well as zygomatic implants. He serves on review boards for multiple peer-reviewed journals and is a diplomate of the American Board of Oral and Maxillofacial Surgery and an honorary member of the American College of Prosthodontists. Dr Bedrossian maintains a private practice limited to implant and oral and maxillofacial surgery in San Francisco, California. Edmond Armand Bedrossian, DDS, MSD, is a board-certified prosthodontist and currently practices in his hometown of San Francisco, California. He received his DDS from the University of the Pacific Arthur A. Dugoni School of Dentistry in 2015 and completed the advanced prosthodontics residency program and received his master’s degree at the University of Washington, where he is currently an affiliate assistant professor. He is a diplomate of the American Board of Prosthodontics and has authored various publications on removable prosthodontics and treatment planning the fully edentulous patient. He has lectured nationally and internationally on implant and prosthetic dentistry. Along with Dr Ryan Mizumoto, he co-founded D365, a social media application providing a networking platform for dental students, residents, and dental practitioners.
Edmond Armand Bedrossian, DDS, MSD, is a board-certified prosthodontist and currently practices in his hometown of San Francisco, California. He received his DDS from the University of the Pacific Arthur A. Dugoni School of Dentistry in 2015 and completed the advanced prosthodontics residency program and received his master’s degree at the University of Washington, where he is currently an affiliate assistant professor. He is a diplomate of the American Board of Prosthodontics and has authored various publications on removable prosthodontics and treatment planning the fully edentulous patient. He has lectured nationally and internationally on implant and prosthetic dentistry. Along with Dr Ryan Mizumoto, he co-founded D365, a social media application providing a networking platform for dental students, residents, and dental practitioners. Lawrence E. Brecht, DDS, received his dental degree from New York University College of Dentistry and completed his prosthodontics and maxillofacial prosthetics residencies at the Veterans Administration Medical Center in Manhattan. Dr Brecht is currently the director of maxillofacial prosthetics at Lenox Hill Hospital, Long Island Jewish Medical Center, and North Shore University Hospital of Northwell Health, the largest hospital system in New York State. In addition, he serves as the director of maxillofacial prosthetics in the postgraduate prosthodontics program of NYU College of Dentistry, where he is an adjunct associate clinical professor of prosthodontics. Dr Brecht has authored multiple articles and chapters on the maxillofacial reconstruction and oral rehabilitation of patients with cancer or craniofacial anomalies and is on the editorial review boards of several well-regarded journals. He serves as the president of the Maxillofacial Foundation as well as NextGenFace Foundation. Dr Brecht currently maintains a private practice limited to prosthodontics in New York City.
Lawrence E. Brecht, DDS, received his dental degree from New York University College of Dentistry and completed his prosthodontics and maxillofacial prosthetics residencies at the Veterans Administration Medical Center in Manhattan. Dr Brecht is currently the director of maxillofacial prosthetics at Lenox Hill Hospital, Long Island Jewish Medical Center, and North Shore University Hospital of Northwell Health, the largest hospital system in New York State. In addition, he serves as the director of maxillofacial prosthetics in the postgraduate prosthodontics program of NYU College of Dentistry, where he is an adjunct associate clinical professor of prosthodontics. Dr Brecht has authored multiple articles and chapters on the maxillofacial reconstruction and oral rehabilitation of patients with cancer or craniofacial anomalies and is on the editorial review boards of several well-regarded journals. He serves as the president of the Maxillofacial Foundation as well as NextGenFace Foundation. Dr Brecht currently maintains a private practice limited to prosthodontics in New York City.


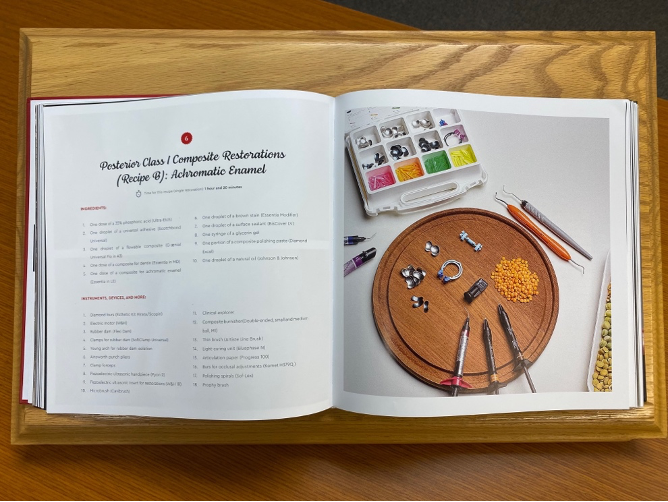
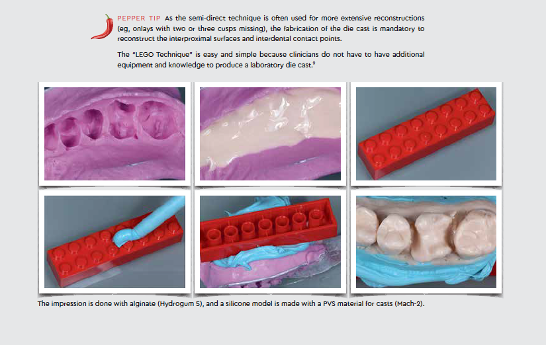
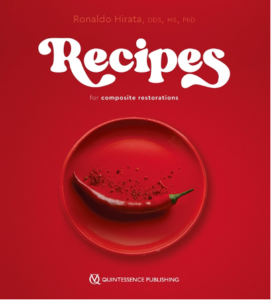
 Ronaldo Hirata, DDS, MS, PhD, finished his 4-year DDS course at the Federal University of Parana in Curitiba, Brazil, in 1995. After completing his degree, he undertook a 2-year operative dentistry specialty at the same university and began lecturing internationally, with a focus on esthetic dentistry. Dr Hirata has now lectured in more than 40 countries and maintains a private practice limited to esthetic dentistry in Curitiba. To improve his scientific knowledge, Dr Hirata finished a master’s degree in dental materials in 2003 at the Catholic University of Rio Grande do Sul, with a research thesis working with glass and polyethylene fibers to improve mechanical properties of composites. His PhD in restorative dentistry at the State University of Rio de Janeiro was completed in 2009, with research focusing on the transmittance, reflectance, and fluorescence of composite resins. In 2012, Dr Hirata undertook a postdoctorate at New York University (NYU) working with plasma application on dentin surfaces and bonding strength analysis. Now, he is Assistant Professor in the Department of Biomaterials at NYU with a secondary appointment in the Department of Cariology. Dr Hirata has published more than 100 papers in English, Portuguese, and Spanish, and his previous books (TIPS, Artes Medicas, 2014; Shortcuts, Quintessence, 2017) were both published in three languages.
Ronaldo Hirata, DDS, MS, PhD, finished his 4-year DDS course at the Federal University of Parana in Curitiba, Brazil, in 1995. After completing his degree, he undertook a 2-year operative dentistry specialty at the same university and began lecturing internationally, with a focus on esthetic dentistry. Dr Hirata has now lectured in more than 40 countries and maintains a private practice limited to esthetic dentistry in Curitiba. To improve his scientific knowledge, Dr Hirata finished a master’s degree in dental materials in 2003 at the Catholic University of Rio Grande do Sul, with a research thesis working with glass and polyethylene fibers to improve mechanical properties of composites. His PhD in restorative dentistry at the State University of Rio de Janeiro was completed in 2009, with research focusing on the transmittance, reflectance, and fluorescence of composite resins. In 2012, Dr Hirata undertook a postdoctorate at New York University (NYU) working with plasma application on dentin surfaces and bonding strength analysis. Now, he is Assistant Professor in the Department of Biomaterials at NYU with a secondary appointment in the Department of Cariology. Dr Hirata has published more than 100 papers in English, Portuguese, and Spanish, and his previous books (TIPS, Artes Medicas, 2014; Shortcuts, Quintessence, 2017) were both published in three languages.